Dry mouth, stomach butterflies, sweaty hands: we all know what stress feels like. But ongoing periods of stress can have a significant impact on your heart health, too.
While it’s normal to feel tense in high-pressure situations, “chronic stress” is the kind of pressure that settles in for the longer haul. It has been described as “a consistent sense of feeling pressured and overwhelmed over a long period of time” – the type of anxiety that can be provoked by something like “a toxic work environment, or caregiving, or being unable to pay your bills.”
And there’s growing evidence that stresses like these can cause actual, physical damage to our hearts. One study in The Lancet, for example, found that people who reported “psychosocial” issues such as high stress and depression were 2.5 times more likely to have a heart attack than those who didn’t. A more recent Swedish study found that being stressed at work was associated with a 48% higher risk of a heart rhythm condition called atrial fibrillation.
If that’s the case, then practising stress management is vital for all of us – but all the more so if you already live with a heart rhythm problem or a heart condition. So how exactly does stress affect the heart? And what can you do, practically, to protect yourself against it?
How Stress Affects Your Heart
When your brain feels stressed, it activates something called the autonomic nervous system (ANS). This is a network of nerves that regulates some of the body’s most basic functions, such as breathing, producing sweat, and the rate at which your heart beats. One way it does this is by releasing chemicals like adrenaline and cortisol into the bloodstream.
These so-called stress hormones are designed to trigger your “fight or flight” reaction. This is useful when it comes to surviving temporary danger – an unexpected confrontation with a bear in Phoenix Park, for example. But it’s much less helpful if your body is exposed to it over a longer period of time. The physical impacts on the heart include:
Increased heart rate
Under stress conditions, the heart contracts more quickly and powerfully than normal. This chronic strain can detrimentally affect the heart’s function and even alter its structure, potentially leading to dangerous adaptations such as left ventricular hypertrophy, a thickening of the heart wall.
Higher blood pressure (hypertension)
The heart pumps blood around the body with more force than normal. This puts the heart under increased strain, and can damage cells in the arteries’ inner lining, reducing their elasticity and allowing plaques to build up and narrow the arteries.
Irregular heartbeats or palpitations
The heart “skips” or adds a beat, or a series of extra beats, which you might experience as a pounding, racing, or fluttering feeling in your chest. Over time, these irregular beats or palpitations could raise the risk of developing a more serious, ongoing heart rhythm problem (see below).
Can Stress Cause Arrhythmias?
While stress isn’t usually the root cause of arrhythmias, it can potentially trigger or aggravate a rhythm problem that’s already present in your heart. Some of the more common heart rhythm conditions that can be affected by stress include:
- Atrial fibrillation (AFib) – When electrical signals in the heart become random or chaotic, causing the heart’s upper chambers to quiver (fibrillate). This results in an irregular heartbeat, which in turn reduces the heart’s pumping efficiency.
- Premature Ventricular Contractions (PVCs) – Where the heart produces extra beats, starting in the lower chambers (the ventricles). This can disrupt the heart’s regular rhythm, causing symptoms like a thumping heart, a fluttering feeling, or the sense that your heart is skipping beats.
Chronic stress also raises the risk of several other types of heart conditions, such as coronary artery disease, heart disease and stroke. It has also been known to trigger a condition called Takotsubo syndrome (“broken heart syndrome”), where the left ventricle becomes enlarged and partially ‘paralysed,’ weakening the heart muscle and causing symptoms that can feel similar to a heart attack.
For a more detailed analysis of the link between stress and heart rhythm conditions, see our recent blog: Can stress cause an arrhythmia?
Recognising the Signs of Stress-Related Heart Symptoms
If your heart was being negatively affected by chronic stress, how would you know? What would it actually feel like?
Like many things in life, people experience and express stress in their bodies in different ways, so the symptoms of extreme stress can vary widely, from headaches and migraines to stomach-related problems like ulcers and bowel disorders.
A heart under stress won’t always offer up obvious clues about what’s going on (in fact, some rhythm-related conditions, such as atrial fibrillation, can occur without any symptoms at all). But if stress does result in symptoms, the more common ones include:
Racing heart
A feeling, or even a physical sensation, that your heart is beating more quickly or more forcefully than normal. Sometimes anxiety simply heightens our awareness of the way our heart is beating. But it can also be a sign that the heart is genuinely beating faster than it should.
Chest tightness
A sense that your chest is constricted or under pressure. Stress can certainly cause discomfort and tightness in the chest, possibly due to tautened chest muscles. Though stress-related chest tightness is usually harmless, it can be a signal that something more serious is going on.
Skipped beats
A feeling that your heart is missing a beat, either occasionally or frequently. Skipped beats are one of the symptoms you might experience with a stress-related palpitation. But they can also be signs of a rhythm issue in the heart.
Feeling faint or dizzy
Dizziness or feeling faint can, of course, be triggered by the brain feeling under extreme emotional pressure. But losing consciousness (or feeling dizzy) is also a symptom of several physical, heart-related problems that need to be investigated.
The bottom line: symptoms are the body’s way of signalling that something isn’t right. So, whether the signals are psychological in nature or rooted in a physical problem with the heart, it’s important to pay attention to any new or unexpected symptoms – especially if you’ve already been diagnosed with a heart condition.
Stress Management Techniques That Help
So if you’re going through a tough period right now, or you’re concerned that stress might be making a pre-existing arrhythmia worse, how can you counteract it?
The good news is that there are some relatively simple things you can do – in some cases right away – to control and mitigate the effects of stress on your heart. As we learn more about the link between stress and heart health, stress management is becoming an increasingly important part of the medical toolkit.
Here are six areas to focus on:
Don’t ignore symptoms
If you get new or unusual symptoms with high stress, it may be time to go for a check-up. Although many heart-related symptoms turn out to be benign, some can indicate a genuine problem within the heart.
Warning signs to look out for include:
- Chest pain that radiates to other areas
- Breathlessness when you wake up
- Reduced tolerance for exercise
- New palpitations (especially if you have a history of heart issues)
- Sudden fainting
We explore these important symptoms in more detail in an article that was published in the Independent: see 5 Heart Symptoms You Shouldn’t Ignore.
Deep breathing and meditation
Slower, more focused breathing helps to normalise the balance between oxygen and carbon dioxide in your blood (CO2 often builds up in times of stress because we take shallower breaths). It also stimulates the vagus nerve – the so-called “rest and digest” branch of the parasympathetic nervous system – to produce a chemical called acetylcholine. This slows your heart rate, lowers blood pressure, and works against the “fight or flight” response.
To practise this kind of breathing, try inhaling for seven seconds, then exhaling for nine seconds, focusing on the exhale as you do so.
The HSE’s Relaxation Tips page has a helpful six-step guide for how to do this.
Exercise and movement
The health benefits of taking regular exercise are legion. Among other things, it improves blood flow and bone strength, strengthens muscles, helps control bodyweight, increases pain tolerance, and even boosts energy levels by stimulating the body to produce more mitochondria inside muscle cells.
In its guidelines for preventing cardiovascular disease, the European Society of Cardiology (ESC) recommends a minimum 150 minutes of moderate activity or 75 minutes of vigorous activity per week.
You can read their detailed advice here: Physical activity for cardiovascular prevention.
Cognitive Behavioural Therapy (CBT)
Mind over matter may be a cliché, but research has consistently proven that adjusting our mental approach to stress can have a profound impact on our physical wellbeing – for instance by reducing the effects of anxiety or depression that often occur alongside a condition like heart failure.
CBT works by identifying unhelpful thoughts, examining the evidence for and against them, and then developing more balanced perspectives and behaviours.
You can find out more about the CBT services available in Dublin here.
Limiting caffeine and alcohol
Both caffeine (a stimulant) and alcohol (primarily a depressant) can influence the stress response, though in different ways. Caffeine has been found to raise cortisol levels in people who are going through mental stress. Excessive drinking raises heart rate, blood pressure and the overall risk of developing an arrhythmia.
Even in normal circumstances, the HSE recommends a maximum of 11 standard drinks per week for women and 17 standard drinks for men (“standard” is one small glass of wine or half a pint of beer). And if that seems surprising, you’re not alone: research has found less than 3% of Irish adults can correctly identify the low-risk guidelines for alcohol consumption.
Better sleep routines
Sleep has a major influence on the body’s ability to regulate and repair itself. Consistently bad sleep, by contrast, is linked to an increased risk of everything from high blood pressure and obesity to heart attacks and strokes.
While most of us struggle to get enough sleep, it’s worth persisting with routines and techniques that are well known to help – particularly if you’re experiencing chronic stress. Avoiding large meals 3 to 4 hours before bed, being more active during the day, and cutting out our old friend caffeine 4-6 hours before sleep time are just some of the better-known examples.
You can find more in the HSE’s Sleep problems – tips and self-help section.
Looking for more stress-busting tips? There are many other ways to manage chronic stress in your own daily life and work.:
- The Irish Heart Foundation has some helpful suggestions in its Stress section
- The HSE’s Stress pages have plenty of recommended resources to try, from CBT apps to mental health support
- The Croí Heart and Stroke Charity has advice and a helpline for people living with or affected by heart disease and stroke.
When to Seek Medical Help
If you’re experiencing frequent palpitations or symptoms that are beginning to affect your daily life, you should speak to a cardiologist – or to your GP, who may refer you to a cardiologist. This is especially crucial if you have an increased risk of cardiovascular issues, such as diabetes or a pre-existing heart rhythm condition.
Some heart-related symptoms should be treated as a medical emergency. Signs of a heart attack can include:
- Chest pain – a sensation of pressure, tightness, or squeezing in the centre of your chest
- Pain in other parts of the body – it can feel as if the pain is travelling from your chest to your:
- arms
- jaw
- neck
- back
- belly
- Feeling lightheaded or dizzy
- Sweating
- Shortness of breath
- Feeling sick (nausea) or being sick (vomiting)
- An overwhelming sense of anxiety (like having a panic attack)
- Coughing or wheezing
Is stress or anxiety becoming a serious problem for you or someone you know? The HSE recommends talking to a GP or mental health professional if you’re finding it hard to cope, if your anxiety is having a negative effect on your day-to-day life, or if your anxiety has been going on for a while or is getting worse. Ask for an urgent appointment if you feel like you are in crisis.
How We Help Patients with Stress-Related Heart Rhythm Problems
Chronic stress can be overwhelming, scary, and sometimes very isolating – particularly when it’s starting to cause issues for your heart health, or if you fear that it might be. But you should never feel trapped by it.
If you’re suffering from significant stress at the moment, or a stress-related rhythm problem, the team at Heart Rhythm Cardiologist are ready to get you the support you need. Call or email us to arrange an appointment with Dr Lyne. He’ll ask you more about your medical history and the symptoms you’re experiencing.
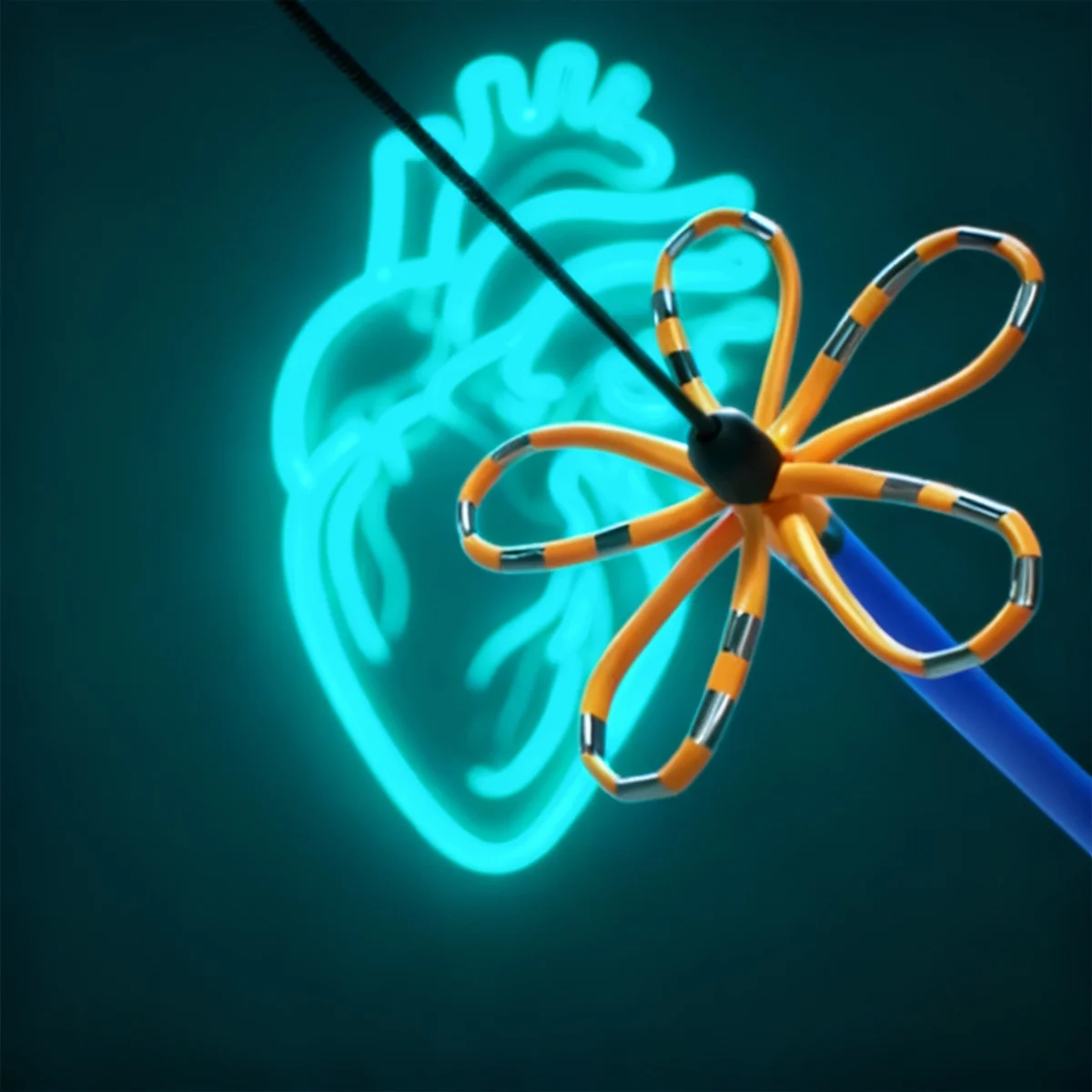
If you need further investigation, we can arrange outpatient cardiac testing for you at one of our private hospitals in Dublin; these include electrocardiogram (ECG) and Holter monitor tests. Once we have your diagnosis, we’ll create a personalised treatment plan for you – including coordinated care with GPs or mental health specialists if needed.
Concerned about how stress may be affecting your heart rhythm? Get in touch with Dr Lyne at Heart Rhythm Cardiologist.
Stress and Heart Rhythm: FAQs
Chronic stress has been described as a consistent sense of feeling pressured and overwhelmed over a long period of time. It can be triggered by life circumstances like a toxic work environment, caregiving responsibilities, or financial difficulties.
Stress activates the autonomic nervous system, which controls basic body functions like our heart rate. This triggers the release of stress hormones like adrenaline and cortisol. While this reaction is useful for surviving temporary danger, prolonged exposure puts significant strain on the heart, including a raised heart rate, higher blood pressure and an increased risk of arrhythmias.
While stress isn't usually the root cause of arrhythmias, it can potentially trigger or aggravate existing heart rhythm problems. Common conditions that stress can influence include atrial fibrillation (where electrical signals become chaotic), premature ventricular contractions (extra beats from the lower chambers).
Common warning signs include a racing heart or a feeling that your heart is beating more quickly or forcefully than normal, chest tightness, and skipped beats where you feel your heart is missing beats. You might also experience feeling faint or dizzy; while this might have a psychological cause, it can also indicate a physical problem within the heart.
There are many very effective techniques for reducing and controlling stress, so it's worth experimenting to see what works best for you. Some of the most popular approaches focus on deep-breathing (which can slow heart rate and lower blood pressure), being more conscious about your activity levels during the day and sleep routines at night, and cutting back on potential stress-enhancers such as caffeine and alcohol.