Cutting-edge pulsed field ablation technology is about to arrive in our clinics in Dublin
Unless you keep a close watch on cardiology journals (which is probably unlikely), you may not have come across the term pulsed field ablation before.
PFA (for short) is a new technology that has been going through clinical trials in Europe and America recently. It’s designed to treat atrial fibrillation (AF), the most common heart rhythm problem. And we’re delighted to say it’s about to become available to patients here in Dublin.
Based on early results, pulsed field ablation has been generating quite a lot of excitement amongst cardiologists. Some experts have described it as a “game changer” and, potentially, as the future of ablation treatment for AF.
So how exactly does it work? Here’s a brief summary.
What does atrial fibrillation do to the heart?
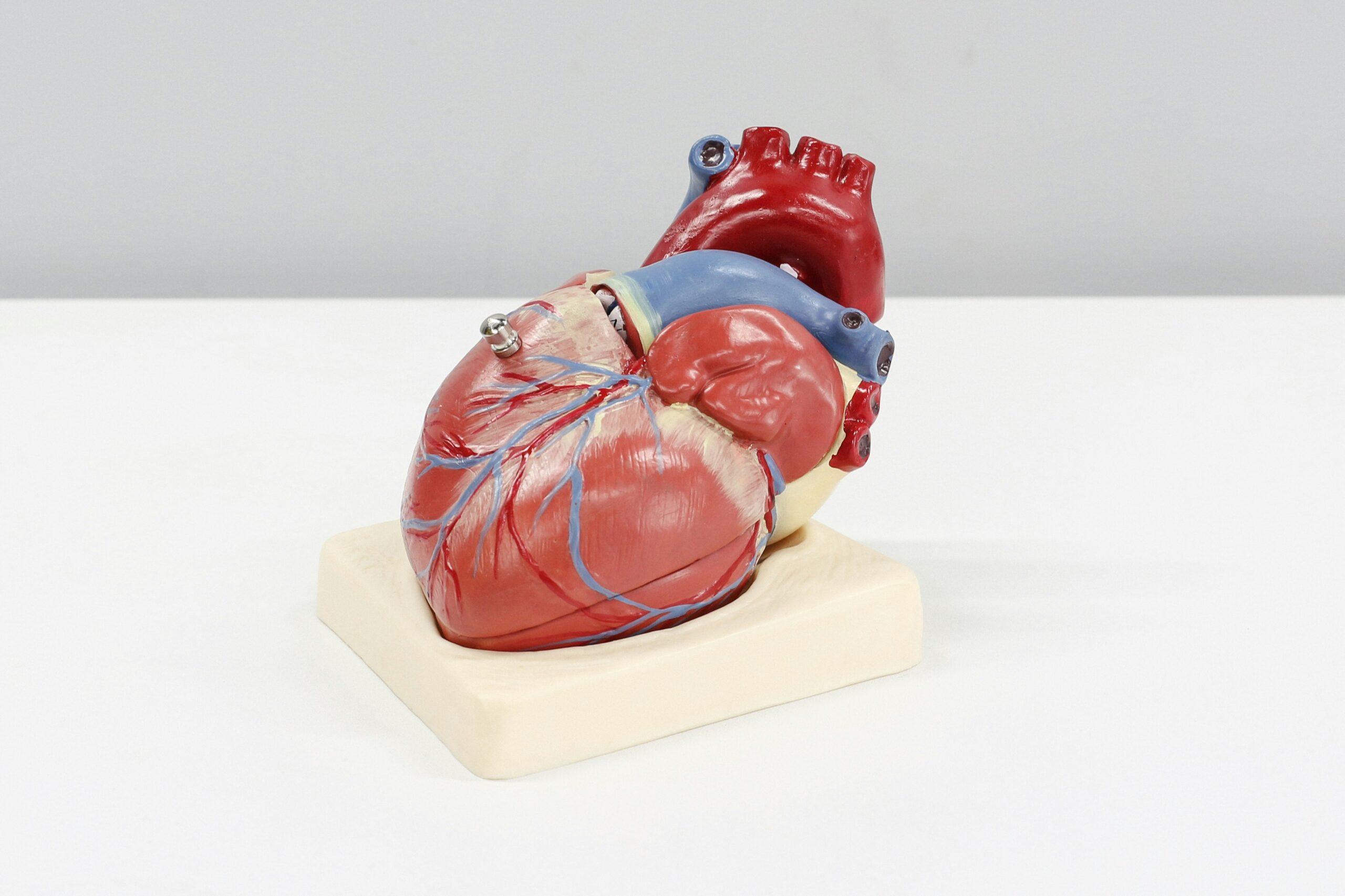
Our heart rhythm is controlled by electrical impulses from the brain. These impulses run from the atria (upper chambers) to the ventricles (lower chambers). In AF, the electrical activity in the atria becomes chaotic. This stops the atria from beating in the normal way, and can cause the ventricles to beat irregularly and often too fast. The result is a range of unpleasant symptoms, from palpitations and shortness of breath to dizziness and fatigue.
How does regular ablation treatment work?
Ablation is a keyhole procedure that’s generally recommended for patients who haven’t responded to other treatments (such as medication) to control their AF. The most common version is catheter ablation, which targets the areas of heart tissue that are generating the rogue electrical pulses. Using a small probe, it heats or freezes the tissue cells to create tiny scars. These scars block and isolate the rogue impulses, stopping the arrhythmia.
What’s different about pulsed field ablation?
Rather than heating or freezing, PFA uses a non-thermal electrical field – generated by two tiny electrodes – to target the problem tissue. The energy pulses create pores in the cell membrane (“electroporation”). The pores are incredibly small: just a nanometre in diameter (for reference, a sheet of paper is around 100,000 nanometres thick). But they have the same effect as thermal energy, scarring the tissue to block the ‘faulty electrics’.
Why is it so promising?
PFA is very precise in the way it ablates the target tissue in the heart. Unlike catheter ablation, it doesn’t need to be in direct contact with the tissue as it creates the scars. In fact, it’s completely non-contact. Its high precision and non-thermal approach mean there’s less risk of damaging surrounding nerves and tissues, such as in the oesophagus, unnecessarily. It also has the ability to create deeper scars (or lesions), which will be very useful in certain arrhythmia cases. Finally, the equipment we’ll be using – the Affera from Dublin-based company Medtronic – comes integrated with 3D mapping to get a precise view of the target area. Though it’s early days for PFA treatment, the initial results are very promising. The hope is that it will lead to even safer and more effective results for patients with AF in the months and years to come.
Useful resources
Interested in reading more about AF and PFA? You may find these resources helpful.
Our website sections on atrial fibrillation and catheter ablation
Pulsed Field Ablation: a new treatment option for AF (Arrhythmia Alliance article)