What’s the best way to treat atrial fibrillation (AFib), the heart rhythm condition that affects more people than any other?
That’s the big question behind the European Society of Cardiology’s new guidelines for the management of atrial fibrillation, one of the most influential publications in international cardiology.
The document, reviewed by some of the world’s leading experts, including Dr Lyne here at Heart Rhythm Cardiologist (whose research is also referenced in the booklet), offers a wealth of new recommendations about how doctors should be diagnosing and treating AFib.
So, what are the latest developments? Here are four of the key takeaways.
Atrial fibrillation is on the rise
The Guidelines warn that the number of AFib patients is going up – though that’s partly because doctors are getting better at diagnosing it. “The prevalence of AF is expected to double in the next few decades as a consequence of the ageing population, an increasing burden of comorbidities, improved awareness, and new technologies for detection,” the paper explains.
CARE is key
The Guidelines also launched a new “care pathway” for doctors called AF-CARE. It stands for Comorbidity and risk factor management (i.e., addressing other health problems that can cause AFib or make it worse); Avoiding stroke and thromboembolism (lowering the risk of blood clots); Reducing symptoms by rate and rhythm control; and Evaluation and dynamic reassessment (meaning “care that adapts to how your AF can change over time, to better prevent complications”).
This comprehensive approach aims to provide more effective and personalised care for AFib patients.
Doctors need to treat the whole patient
There’s a new focus on treating the patient “as a whole.” That means, for example, “managing [a patient’s] diabetes, their high blood pressure, their obesity, [and] giving them information about physical activity,” Dipak Kotecha, one of the report’s authors, told the journal TCTMD. “All of that stuff is not only going to help them… but also prevent the atrial fibrillation from recurring. And if [the doctor is] giving them treatments, it’s going to make the treatments work much better.”
Patients need to be more involved in decisions
Although modern treatments for AFib are better than ever, managing the condition can mean significant lifestyle changes. For these to stick, the patient needs to be fully behind them. “You should expect to be involved in the decisions made, including what treatments you receive,” say the authors. “This should involve a broad range of healthcare staff, including nurses, pharmacists and specialist doctors, led by your GP or cardiologist.”
Read the patient version of the Guidelines
The full ESC Guidelines are meant for doctors rather than the public. Fortunately, the authors have also created a slimmed-down leaflet in ordinary language. Designed to help patients “take an active part in the care they receive for their AF and understand why they are receiving a range of different treatments,” it’s an excellent summary guide to how atrial fibrillation works. Highlights include:
- What atrial fibrillation is
- Common symptoms of AFib
- Learning to live with atrial fibrillation
- What should happen at your initial evaluation
- The risk of blood clots with AFib
- The different blood thinners and heart tablets available
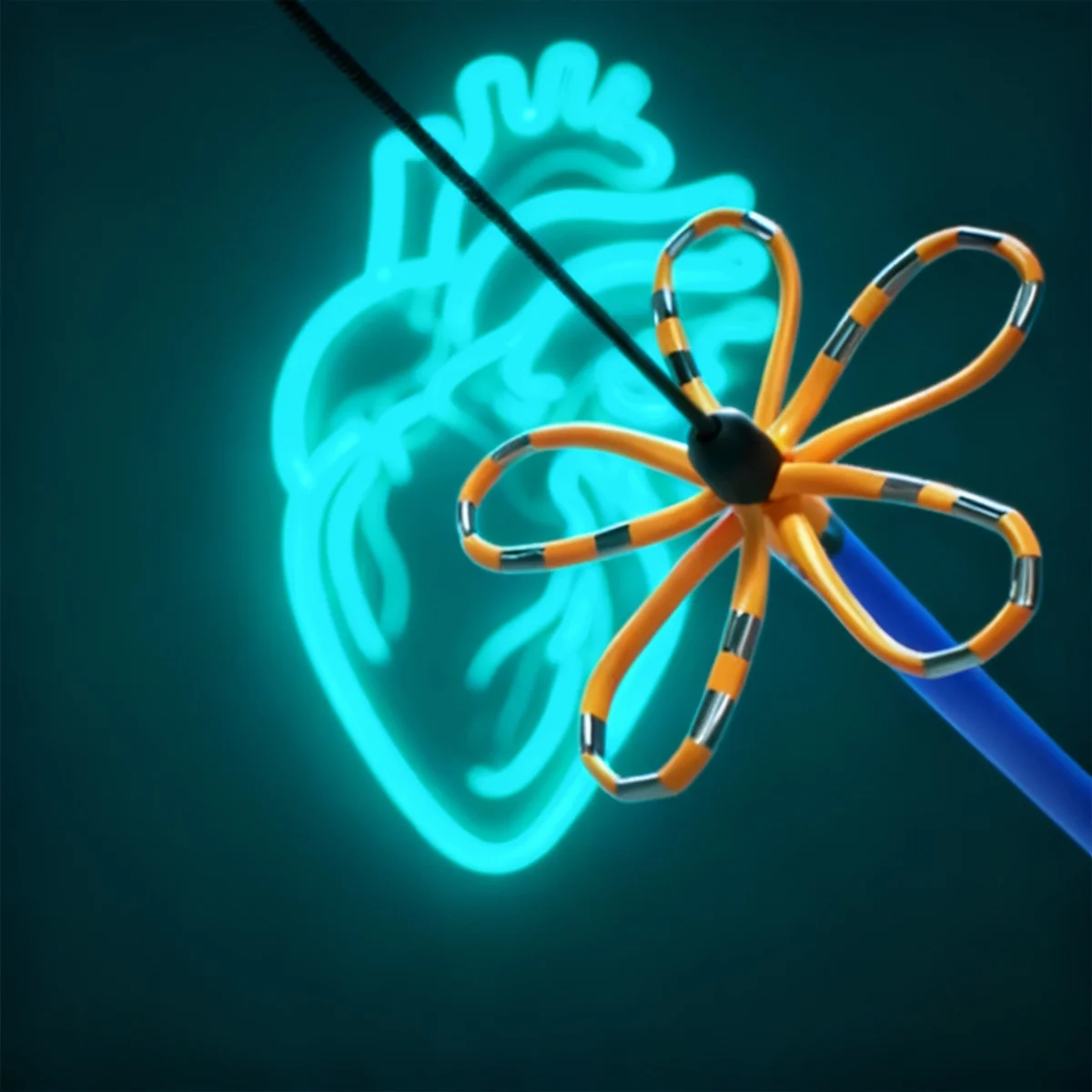
- The main procedures for AFib, including cardioversion and catheter ablation
We highly recommend you read this patient version to stay informed and prepared.
ECG (Electrocardiogram): FAQs
AFib is an irregular and often fast heart rhythm that increases the risk of stroke and other complications.
The AF-CARE pathway focuses on managing comorbidities, avoiding stroke, controlling heart rate and rhythm, and reassessing care over time.
Managing conditions like diabetes and high blood pressure helps prevent AFib from getting worse and makes treatments more effective.
Patients should actively participate in treatment decisions alongside their healthcare team, which includes specialists and their GP.
Common procedures include cardioversion, which resets the heart’s rhythm, and catheter ablation, which targets the areas causing abnormal rhythms.