You may have read recently that Dr Lyne’s Beacon Hospital department has been asked to join a ground-breaking global study into a new technology for heart failure patients.
This is encouraging for Beacon, of course – the hospital is one of only 12 cardiac centres of excellence in the world to be selected for the trial, and the only centre in Ireland. If the results are successful, though, it has the potential to transform the way we perform Cardiac Resynchronisation Therapy (CRT), one of our most important tools in the fight against heart failure.
So what exactly is the trial aiming to do? Here’s a brief explainer.
What is heart failure?
Heart failure is what happens when a heart is no longer able to pump enough blood around the body. This sometimes occurs because faulty electrical signals disrupt the heart rate, causing the lower chambers of the heart (the ventricles) to stop working efficiently together.
How can you tell if someone has heart failure?
We can detect the abnormal signals using an ECG, a simple test for checking the heart’s rhythm and electrical activity. These signals can produce very distinctive patterns during the test. One particular pattern is known as a “wide QRS”. Patients with a wide QRS are the key focus of this study.
How do you normally treat these patients?
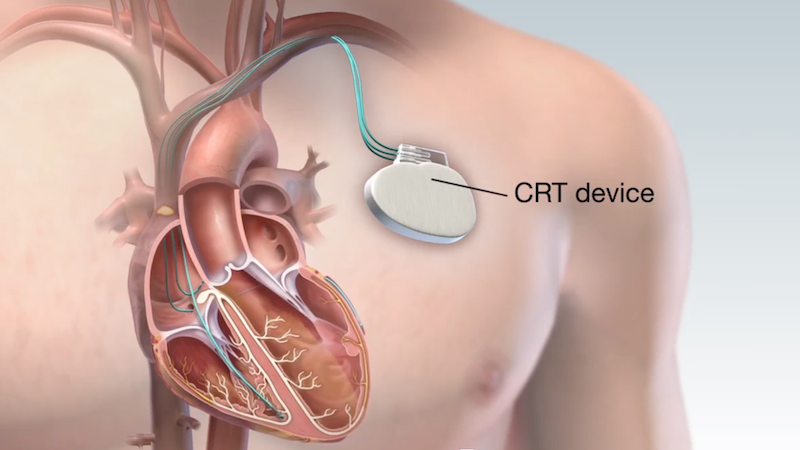
The standard treatment is Cardiac Resynchronisation Therapy (CRT). This involves placing a special type of pacemaker in the patient’s chest to continuously monitor their heart rate. If the device detects an irregularity, it can emit a series of pulses to make the ventricles contract normally (i.e. “resynchronise” them). Because the pulses target both sides of the heart, we call this “biventricular pacing”.
What does the new treatment do?
Research has shown that patients with a wide QRS don’t always respond so well to traditional biventricular pacing. In some cases, they can still feel unwell after their device has been implanted. Recently, though, scientists have discovered an alternative approach that targets another part of the heart’s internal wiring system, with a different kind of pacing.
How does it actually work?
Unlike biventricular pacing, it focuses on the “left bundle branch”, one of the two key pathways that distribute electrical signals evenly through the heart. It does this by sending pulses down a tiny lead into the left ventricle to correct the pacing. Researchers are calling this the CSPOT configuration (full name: Conduction System Pacing Optimized Therapy).
What could CSPOT mean for heart failure patients?
The hope is that it will produce better outcomes for patients with wide QRS who need CRT treatment – a substantial group of people. By working with the heart’s intrinsic conduction system, scientists hope CSPOT will be able to synchronise patients’ ventricles more efficiently and improve the way they pump. That’s what the trial is focusing on – we hope to see evidence that CSPOT leads to even better results for this patient group.
Could I take part in the trial?
If you’ve been diagnosed with heart failure and been told you’ll need to have either a “CRT-D” or a “CRT-P” type pacemaker then, yes, you could potentially take part in the study. We are now actively looking for patients to get involved. You will need to be 18 or older, and able to provide your written informed consent to take part in the trial.
If you’d like to find out more, please contact us on [email protected]. We’ll be pleased to explain the details and see if you might be suitable for the trial.
Interested in reading more about the CSPOT trial? See these links at the US National Library of Medicine and the NHS in the UK.